Last Updated on: 4th December 2024, 05:12 pm
Disorders of the Temporomandibular joint (TMJ): How to cure TMJ permanently
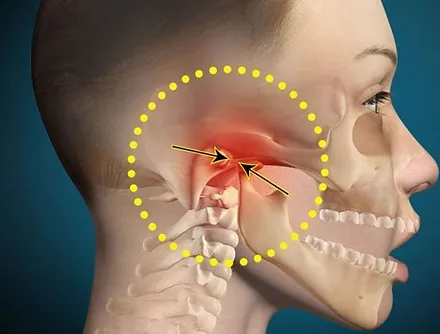
The jaw is a hinge joint called the temporomandibular joint. There is one on each side of the skull.
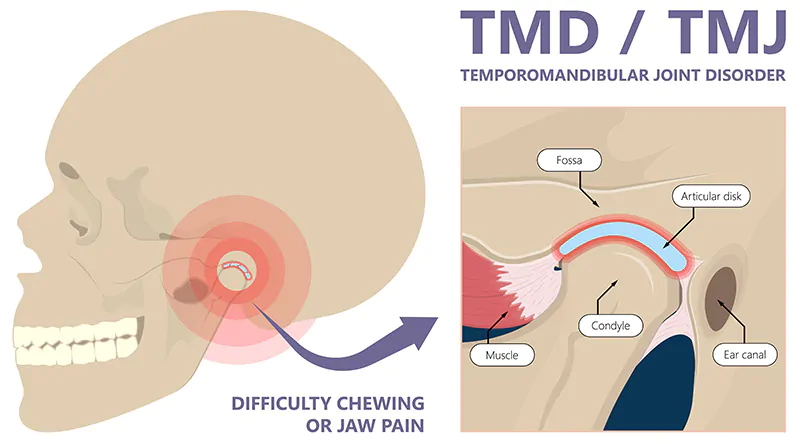
Temporomandibular disorders (TMD) are a group of musculoskeletal and neuromuscular conditions that affect the complex temporomandibular joint, the surrounding musculature, and the bony components. They affect the jaw and the surrounding muscles and ligaments that control it.
The most common symptoms may be jaw pain, ear pain, headache, facial pain, mild clicking of the jaw, and difficulty opening the mouth. TMD affects up to 15% of adults, with a higher proportion between 20 and 40 years of age. There are different ways to treat it, based on the medical evaluation from medications and therapies to surgical procedures.
What is TMJ?
The temporomandibular joint (TMJ) is the joint that connects the lower jaw to the skull. It is located on both sides of the face in front of the ears. Together with the muscles, these joints help with chewing and speaking.
What are Temporomandibular Joint disorders (TMD or TMJD)?
Temporomandibular joint disorders, abbreviated as TMD or TMJD, refer to any pain and dysfunction of the jaw joints or the muscles around them.
According to the National Institute of Dental and Craniofacial Research, approximately 10 million Americans are likely to have this disorder; it is more common among women than men.
There are three main classes of temporomandibular disorders:
- Joint disorders, including disc disorders
- Disorders of the muscles used for chewing (masticatory muscles)
- Head pain associated with the disorder
These disorders can cause:
- Tenderness in the joint
- Facial pain
- Difficulty moving the joint
More classifications of TMD syndrome published in the American Academy of Family Physicians provide expanded, specific information.
What are the symptoms and causes of temporomandibular joint disorder (TMD or TMJD)?
Some things that make TMJ worse:
Different types of arthritis, such as rheumatoid arthritis or osteoarthritis
- Clenching of teeth
- Grinding of teeth
- Certain connective tissue diseases affecting the temporomandibular joint
- Prolonged stress
- Female hormones: This theory is under study; it indicates that estrogen may play a role in the development of TMD
Causes of TMJD
In the temporomandibular joint, various bones interact. They are covered with cartilage and separated by a small disc that absorbs the shock, making the movements smooth.

Potential causes of TMD:
- Injuries to the teeth and jaw, such as dislocation
- Dental problems, such as clenching, grinding (bruxism), misalignment, or incorrect bite (malocclusion)
- Poor posture (such as keeping your head forward all day while looking at a computer strains the muscles of the face and neck)
- Autoimmune diseases
- Inflammatory conditions such as arthritis
- Infections
- Trauma
- Stress
- Joint erosion
- Growth disorders
Symptoms of TMJD
It is necessary to know that the temporomandibular joint can generate noises without pain. It is completely normal and does not require treatment. However, some symptoms should be evaluated by a doctor since they could be an indication of a temporomandibular disorder:
- Pain or discomfort in the muscles when chewing or biting or in the jaw joint (most common symptom)
- Pain spreading to the face, neck, and/or shoulders
- Jaw stiffness
- Limited movement that impairs or locks the jaw
- Painful clicking, popping, or grinding noise in the jaw joint when opening or closing the mouth.
- Ringing in the ears or tinnitus, hearing loss, or dizziness
- Change in the way the upper and lower teeth fit together
- Headache and earache
- Intense facial pain in the face
- Feeling of tiredness in the face
- Swelling on one side of the face
- Toothache
- Vertigo
These symptoms can appear on one or both sides of the face. Other factors that could make TMJ symptoms worse are poor diet and a lack of sleep.
Treatment of temporomandibular joint disorders (TMD or TMJD)

Disorders of the temporomandibular joint can be difficult to diagnose. There is no protocol that indicates specific steps. Treatment is simply based on the findings of the patient’s clinical history and a physical examination since the causes and symptoms are not always exact. Your dentist or doctor will ask several questions to make a detailed physical evaluation, following.
- X-ray
- CT scans
- MRI ( to determine if something is wrong with the structure).
You may be referred to a specialist who can diagnose your situation. In any of these scenarios, you may require treatments in stages or only one, depending upon the diagnosis or other health conditions present.
Approximately 5% to 10% of patients require treatment for TMD, while 40% of patients have spontaneous resolution of symptoms. However, the multidisciplinary approach is most favorable for successful treatment.
Lifestyle changes and self-care

Recommended self-care treatments may reduce jaw movement:
- Soft diet to calm joint inflammation
- Learn how to gently stretch, relax, or massage the muscles around your jaw. Your provider, dentist, or physical therapist can help you with this.
- Avoid actions that cause symptoms, such as yawning, singing, and chewing gum
- Apply hot or cold wet compresses to your face
- Learn techniques to reduce stress
- TMJ pain relief exercises several times each week should help increase your ability to manage the pain
- Have a bite analysis
Non-surgical treatments
When simple management and good habits are not enough, and your doctor or dentist diagnoses a specific temporomandibular disorder, he or she may recommend one or more of the following treatments:
a. Therapies
The goal of physical therapy is to maintain, improve, or restore movement and physical function. There are several types:
- Oral splints or mouth guards (occlusal appliances): People with jaw pain may benefit from a soft or firm device inserted over the teeth. It helps with malocclusion, relieving pain and reducing grinding.
- Physical therapy: tmj exercises to stretch and strengthen the jaw muscles may be indicated, or other treatments such as ultrasound, moist heat, and ice.
- Psychological counseling: Cognitive-behavioral therapy seeks to identify and change negative thought patterns as well as provide coping strategies. The idea is that education and counseling will help you understand the factors and behaviors that aggravate the pain so you can avoid them.
- Other: acupuncture, meditation, and biofeedback (using electronic instruments to detect areas of stress and tightness in your body).
b. Medications Medications
Medications may be prescribed to help with pain management. They may be available over the counter (OTC) or require a prescription:
- Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, naproxen, and aspirin
- over-the-counter muscle relaxants
- Prescribed corticosteroids, such as prednisone
- Antidepressants, anticonvulsants, and opioids, among others, may be prescribed.
Surgical and other treatments

Surgery is indicated if all previous options have been ruled out according to the diagnosis or because the problem does not subside. If there is no pain relief with other treatments, the following procedures may be considered:
a. Botox: Botulinum toxin injections can relieve pain from jaw muscle tension.
b. Injections: Doctors may inject corticosteroids directly into the affected joint to reduce pain and swelling.
c. Arthrocentesis: This procedure removes debris and inflammatory byproducts from the joint by flushing the joint with fluid through tiny needles.
d. Arthroscopy: This procedure uses a small, thin tube (arthroscope) to check, diagnose, and treat the cause of TMJ. The procedure may change the position of the cartilage disc, improve joint surfaces, and treat scarring.
e. Open joint surgery (arthrotomy): Doctors use this surgical procedure to repair, replace, or remove parts of the TMJ, but it is more invasive than the other treatments.
Since temporomandibular joint disorders have multiple causes, it is possible to cure them if the exact cause is known and the patient’s response is favorable to the indicated treatments. However, to avoid this disorder in the first place, it is recommended to take into account the above recommendations for better personal care habits. Integrating them into your lifestyle should help reduce the condition, and it may even disappear on its own.
Contact us
If you have any questions about this or other topics, you can contact us at Channel Island Family Dental as well as our Facebook page. We look forward to your visit, and we will make a timely diagnosis. Our dentists in Oxnard, Saint Paula, Venture, Newbury Park, and Port Hueneme will be able to guide you toward the best treatment to take care of your health and give you back your best smile.
Bibliography
- Maini K, Dua A. Temporomandibular Syndrome. [Updated 2022 Apr 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan, consulted on: Sep 21, 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551612/
- Gauer, Robert, M.D.; Semidey, Michael, DMD. Diagnosis and Treatment of Temporomandibular Disorders. Am Fam Physician. 2015;91(6):378-386. American Academy of Family Physicians. Consulted on: Sep 21, 2022. Available from: https://www.aafp.org/pubs/afp/issues/2015/0315/p378.html#article-comment-area
- National Institute of Dental and Craniofacial Research. TMD (Temporomandibular Disorders), NIDCR. Publishing; 2022 Jan, consulted on: Sep 21, 2022. Available from: https://www.nidcr.nih.gov/health-info/tmd
- Kapner, Michael, DDS; Zieve, David, MD. TMJ disorders. National Library of Medicine, Medline Plus. Review on Jan 24, 2022, consulted on: Sep 21, 2022. Available from: https://medlineplus.gov/ency/article/001227.htm
- Tee-Melegrito, Rachel; Frank, Christine DDS. How to treat temporomandibular joint (TMJ) disorders. Medical NewsToday. Review on Mar 16, 2022, consulted on: Sep 21, 2022. Available from: https://www.medicalnewstoday.com/articles/tmj-treatment6
- Burke, Darla; Martinez, Kevin MD Temporomandibular Joint (TMJ) Disorders. Healthline. Review on Mar 16, 2022, consulted on: Sep 21, 2022. Available from: https://www.healthline.com/health/tmj-disorders
- Mayo Clinic Staff. TMJ disorders. Mayo Clinic. Review on Dec 28, 2018, consulted on: Sep 21, 2022. Available from: https://www.mayoclinic.org/diseases-conditions/tmj/diagnosis-treatment/drc-20350945.
- Cleveland Clinic medical professional. Temporomandibular Joint (TMJ) Disorders. Cleveland Clinic. Review on Jun 21, 2018, consulted on: Sep 21, 2022. Available from: https://my.clevelandclinic.org/health/diseases/15066-temporomandibular-disorders-tmd-overview














